Medical contribution by Benjamin S. Harris, M.D., M.P.H.
Benjamin S. Harris, M.D., M.P.H., is board certified in obstetrics and gynecology (OB/GYN) and board eligible in reproductive endocrinology and infertility (REI). Passionate about educating patients and helping them understand the concepts underlying their unique set of reproductive circumstances, Dr. Harris sees patients at SGF Richmond’s Stony Point and Henrico Doctors’ – Forest location, as well as SGF Jones Institute in Norfolk.
During the in vitro fertilization (IVF) process, there are many reasons patients and their physicians may choose not to do a fresh embryo transfer. After an egg retrieval, any embryos that were created could be frozen for later use. Then, when you are ready, an embryo can be thawed and transferred to the uterus during a frozen embryo transfer (FET).
Dr. Benjamin S. Harris, who sees patients at SGF Richmond’s Stony Point and Henrico Doctors’ – Forest locations, answers frequently asked questions about FETs.
What is a frozen embryo transfer (FET)?
A frozen embryo transfer (FET) is a cycle in which the frozen embryos made during the IVF process are thawed and are then transferred back into uterus.
When can I do an FET cycle?
Frozen embryos remain viable well over 10 years or more after the initial freeze. You may do an FET cycle following an unsuccessful fresh IVF cycle. Or you and your physician may not have done a fresh transfer to begin so that you could ensure your body was ready for an FET.
What is the typical FET process?
A FET cycle will take approximately 6 to 8 weeks. A cycle typically begins with 2 to 4 weeks of daily birth control pills to suppress the normal ovarian cycle, as it would lead to ovulation. After the course of birth control, you will need a baseline assessment involving bloodwork and ultrasound. Depending on the test results, your physician may instruct you to begin estrogen (pills or patches), oral medication (such as Femara), or injections (such as FSH) to build the uterine lining.
After a designated period of time on the hormonal medication, you will return for bloodwork and a transvaginal ultrasound lining check. If the lining check demonstrates that your hormone levels are appropriate and your endometrial lining has thickened, your physician will likely instruct you to add daily injections or vaginal suppositories of progesterone to your medication regimen. Your nurse will then confirm an FET date and you will come in for your transfer several days later. Estrogen and progesterone supplementation continue after the transfer. Typically, a blood pregnancy test is checked 10 days after the embryo transfer. If you are pregnant, then hormone supplementation will continue until 10 weeks. If you are not pregnant, then your provider team will provide instructions to discontinue supplements in preparation for another cycle.
What are the success rates for frozen embryo transfers?
The success rates of an FET cycle are comparable to fresh IVF cycles — and can often result in a higher success rate because of the opportunity to optimize the lining of the uterus before implantation and progesterone levels, among other reasons. Both fresh and frozen cycles have the same primary indicator for success: the maternal age at the time of embryo freezing.
Many patients wait several years between the initial freeze of their embryos and attempting a subsequent FET cycle. Any patient, no matter the amount of time between embryo freezing and thawing, can expect nearly the same potential for success as they would expect with a fresh IVF cycle.
What are the benefits of frozen embryo transfers over a fresh (stimulated) cycle?
- Genetic testing
- A major benefit of FETs is that it allows for preimplantation genetic testing to take place. Genetic testing can look for chromosomal abnormalities that may lead to miscarriage or genetic disorders.
- Less medication
- Instead of stimulation medication, patients use estrogen and progesterone to thicken the lining of their uterus in preparation for the embryo transfer to allow implantation. Since the stimulation phase was done in a prior cycle, there is also no egg retrieval requiring anesthesia.
- Less stress
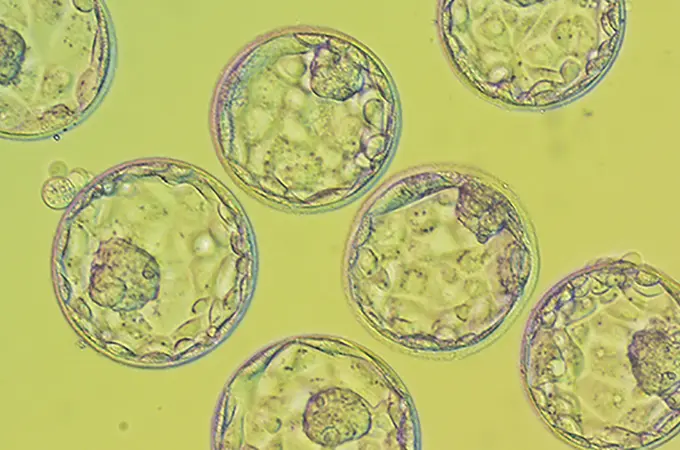
- FET cycles are often less stressful than fresh cycles because factors like stimulation response, egg development, and embryo growth were considered during the fresh cycle. Shady Grove Fertility only freezes high quality blastocyst-stage embryos, giving patients a significant chance of success with an FET cycle. Cycles are also more predictable with fewer cycle cancellations.
How do I schedule an FET?
If you’re ready to proceed with a frozen embryo transfer, contact your local Shady Grove Fertility office and set up an appointment with your physician and nurse to discuss a potential FET cycle. During this time, they will review your records with you to ensure the necessary medical testing and screening is current.
Editor’s Note: This post has been updated for accuracy and comprehensiveness as of November 2023.