In Vitro Fertilization (IVF)
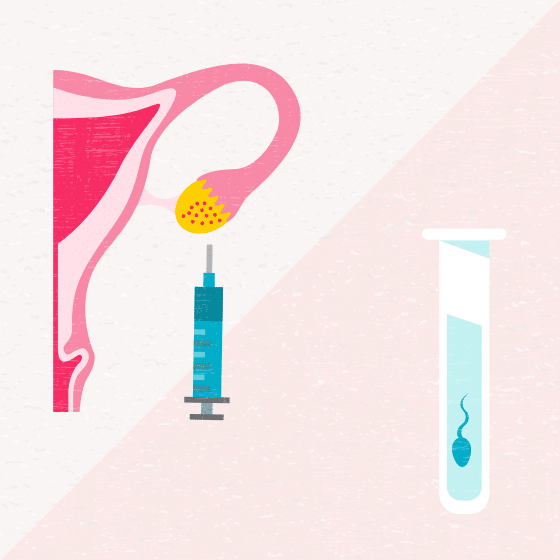
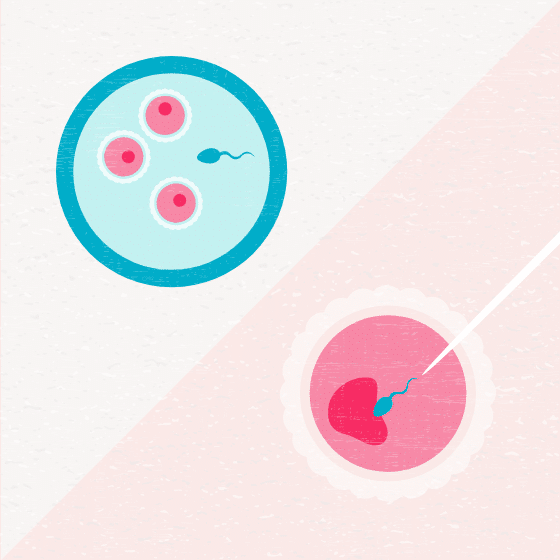
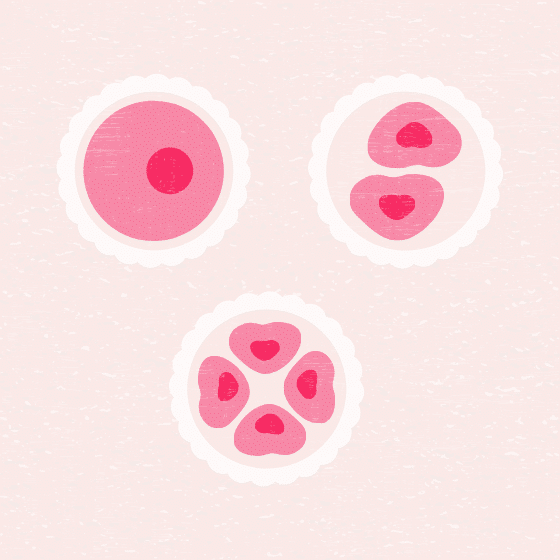
In vitro fertilization (IVF) is a procedure in which a physician will remove one or more eggs from the ovaries that are then fertilized by sperm inside the embryology laboratory. IVF is the most successful treatment you can do using your own eggs and sperm (or donor sperm). IVF has become mainstream and widely accepted, and continues to grow due to significant technological advances.
Common indicators for IVF treatment
Once diagnostic testing is complete, your physician will review your treatment options. Many patients are surprised to learn that IVF is not their only treatment option. However, IVF would be the first line of treatment for patients with the following conditions:
Patients with other diagnoses may start with basic, ‘low-tech’ treatments like hormone therapies or IUI and then transition to IVF if needed. However, with most of the more basic treatment options, data shows that after three to four treatment cycles, success rates begin to decline sharply. By moving to IVF treatment, a couple increases their chances of success dramatically. Some additional diagnoses for which IVF treatment can improve the chances of success include: advanced age, ovulatory disorder, genetic abnormalities, and unexplained infertility.
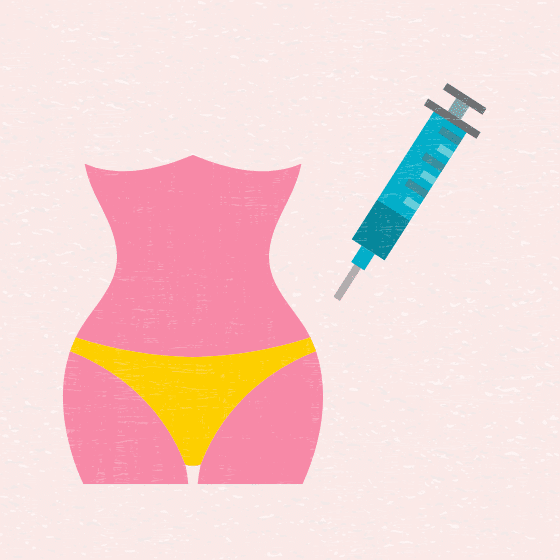
IVF process
In a normal ovulation cycle, one egg matures per month. The goal of an in vitro fertilization (IVF) cycle is to have many mature eggs available, as this will increase your chances of success with treatment. In order for there to be more than one egg available, stimulation of the ovaries needs to occur. It’s important to note that the eggs being stimulated would have grown or died that month, so stimulating the ovaries does not deplete eggs for the future. This is a common question that patients ask, so rest assured.
Success rates
Our state-of-the-art laboratories are at the heart of SGF, offering unparalleled expertise and advanced treatments in embryology, andrology, and endocrinology. Explore our labs.
Note: SGF’s locations in California, North Carolina, and Orlando are new and do not yet have success statistics. Please note a comparison of clinic success rates may not be meaningful because patient medical characteristics, treatment approaches, and entry criteria for ART may vary from clinic to clinic.
Cost of IVF
At Shady Grove Fertility, we understand the financial considerations that go into the decision to begin—or continue—fertility treatment. As part of our efforts to make treatment more affordable, we participate with a wide network insurance providers. While you may have some form of insurance coverage for treatment, or live in a location that has coverage provided by mandate, we recognize that there are many without sufficient coverage or insurance benefits. With that in mind, we developed exclusive financial programs to help ease the cost of treatment, including our Shared Risk 100% Refund Program for IVF or donor egg treatment.
Our Shared Risk 100% Refund Program financially ensures you against the risk of not being successful. We only earn our payment when you take home a baby. In this program, you will pay a flat amount that covers the medical cost of up to six cycles of IVF treatment. More than 80% of applicants qualify for the Shared Risk 100% Refund Program. Eligibility and cost are determined by your age as well as your ovarian, uterine, and sperm function.
The flat fee for the Shared Risk 100% Refund Program also includes the cost of vitrification (flash-freeze technology) and unlimited frozen embryo transfers (FETs) from your qualified cycles. If you do not take home a baby as a result of your cycles, or the transfer of any frozen embryos, or you choose to withdraw from the program before the end of your remaining cycles, we will refund 100 percent of the deposit*, preserving your resources for other family-building options.
* Some exclusions apply.