Intrauterine Insemination (IUI)
Intrauterine insemination (IUI) is one of the simpler, low-tech treatments for infertility and the starting point for many individuals and couples who are having difficulty with conception on their own.
Low-tech fertility treatments like IUI aim to develop one to four eggs, with fertilization taking place within the patient’s body instead of in the laboratory setting.
Common indicators for IUI
Patients who have been diagnosed with unexplained infertility, mild male factor infertility, a cervical factor, or irregular or absent ovulation are often good candidates for IUI.
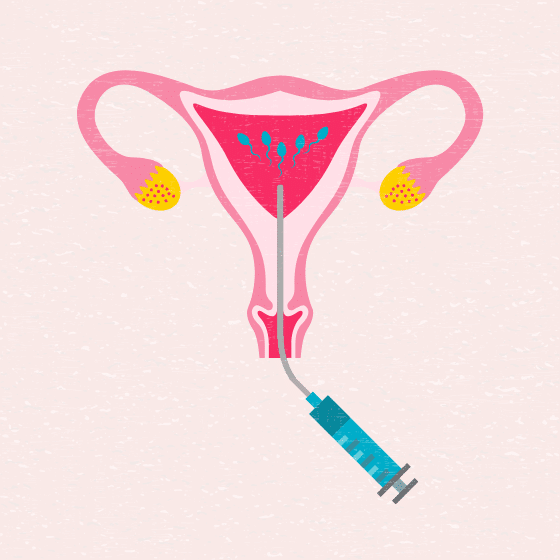
The goal of this treatment is to increase the number of sperm that reach the Fallopian tube and subsequently increase the chance of fertilization. IUI provides the sperm an advantage by giving it a head start but still requires the sperm to reach and fertilize the egg on its own. Depending on your fertility diagnosis, IUI can be coordinated with your normal cycle or with fertility medications.
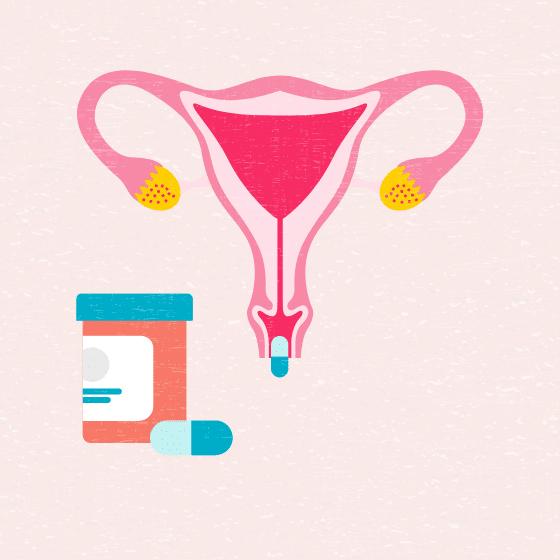
A physician may also recommend IUI in cases where a woman or couple needs donor sperm. Before you and your doctor make the decision about whether or not IUI is right for you, you will undergo standard infertility testing.
Intrauterine insemination (IUI) process
Success rates
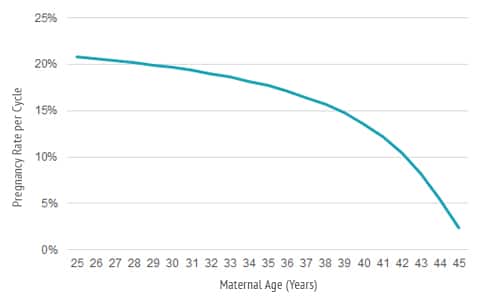
Natural rate of conception varies from 5 to 25 percent based on maternal age
For couples who have no difficulty achieving a pregnancy, the natural chance of pregnancy per month of ovulation is largely dependent on the age of the woman. For women in their early 30s or younger, the natural pregnancy rate is about 20 to 25 percent per cycle. This drops off significantly through her mid-to late-30s; by her early 40s, the chance of pregnancy is about 5 percent per cycle. This age-related decrease is primarily due to a decline in the quality of the eggs within the ovaries.
Intrauterine insemination pregnancy rates by age
For most couples having difficulty achieving a pregnancy their chance of achieving a pregnancy is not zero, it is just lower than the average rate of conception—unless both Fallopian tubes are completely blocked, there is no sperm, or the woman never ovulates. Ovulation induction (or superovulation) with IUI helps patients to achieve pregnancy rates closer to the natural per cycle chance of pregnancy for women in their age group who do not have infertility (see fig 1).
Since the chance of pregnancy per treatment cycle is modest, it may take more than one cycle of IUI treatment in order to achieve a pregnancy. However, after three to four cycles of IUI treatment, if pregnancy has not occurred, it may be advisable to move to more advanced treatments such as in vitro fertilization (IVF).
Because the chance of pregnancy with IUI is low for women over the age of 40, we generally recommend fewer IUI cycles before progressing to IVF. After 40, patients should consider IVF earlier in the treatment timeline.
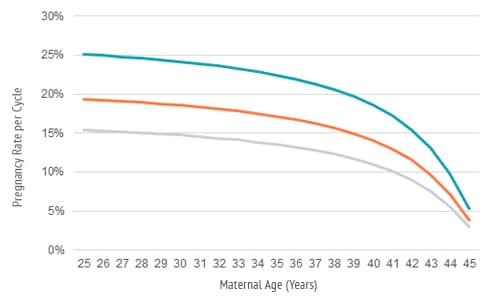
Intrauterine insemination pregnancy rates by diagnosis
In addition to age, a couple’s prognosis for success with IUI depends on their diagnosis (see figure 3). IUI is most successful in couples where the primary cause of infertility is an ovulatory problem such as polycystic ovary syndrome (PCOS). In these cases, the treatment comes closest to restoring the natural per cycle pregnancy rate.
For several reasons IUI is also quite successful for the treatment of mild male factor or unexplained infertility, although the success rates are slightly lower than for those couples where ovulatory dysfunction is the only problem.
Intrauterine insemination is less successful if the cause of infertility involves decreased egg quality, diseased Fallopian tubes, or endometriosis. IUI treatment cannot improve the quality of the eggs within the ovaries or repair damaged anatomical structure. As with advanced age, it may be advisable to move to IVF earlier in the treatment timeline with these diagnoses.
The Fallopian tubes are the site for fertilization before the embryo makes its way to the uterine cavity for implantation. If the Fallopian tubes are damaged, fertilization may not occur. If one Fallopian tube is blocked, it may be due to inherent disease involving both Fallopian tubes; even if the other Fallopian tube is open, it may not be able to provide the appropriate nurturing environment for fertilization and early embryo growth to take place.
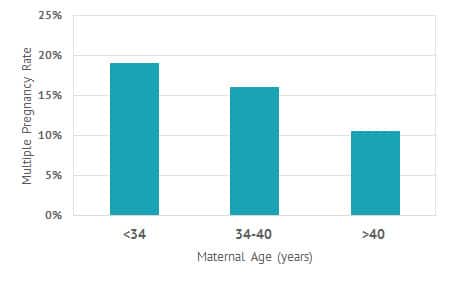
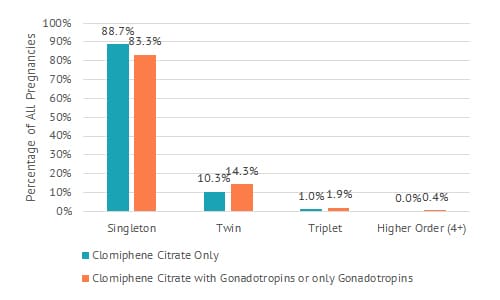
Intrauterine insemination and multiple pregnancies
A major concern for couples undergoing any fertility treatment is the risk of a multiple pregnancy. Shady Grove Fertility pays close attention to patients undergoing stimulation by closely monitoring follicular development to keep the multiple pregnancy rates low (see fig. 4).
FAQs
Learn more about IUI
Patient Story
Dani & Corey
Patient Story