
For patients who are new to either fertility treatment or egg freezing for fertility preservation, the embryology laboratory can be an unfamiliar place. To begin what is embryology and how is the lab different from any other clinical lab? Embryology is the branch of biology and medicine concerned with the study of embryos and their development. An embryo represents the earliest stages of development; the undifferentiated beginnings of a baby, from the point of conception to the 8th week of pregnancy.
The embryology labs at Shady Grove Fertility are vast and awe-inspiring, full of state-of-the-art equipment where cutting-edge scientific procedures help to make patients’ dreams of a family become reality. It is where eggs are frozen for future eggs, where eggs and sperm come together, where embryologists perform genetic screening, and so much more.
Quality Control Inside the Embryology Lab
One of the most important aspects of a well-run embryology laboratory is quality control. At SGF, we have demonstrated exemplary performance when it comes to quality control. The SGF embryology laboratories are accredited by The Joint Commission, and the Ambulatory Surgical Centers are accredited by the Accreditation Association for Ambulatory Health Care, Inc. (AAAHC). These accreditations symbolize excellence, experience, and professionalism—qualities we embrace on a daily basis. Our protocols to ensure quality are numerous and leave zero margin for error.
We have redundant safeguards and quality control protocols in place at every step of the process. From heated work stations that simulate the in vivo (Latin for “within the living”) environment to anti-vibration tables that prevent harm to specimens should the table be jostled, the labs at SGF are state-of-the-art, ensuring the best possible success rates for patients. We even have an air filtration system on the roof that is roughly the size of a city bus. This system supplies carbon and HEPA-filtered clean air to the lab and operating room (OR).
The Top 6 Procedures Happening in the Embryology Lab
- Egg Retrieval
Before the time of egg retrieval, patients have already undergone ovarian stimulation with regular monitoring from their physician. In the lab, before any egg retrieval can begin, the embryologist must perform identity verification. Multiple times throughout every procedure performed in the lab, the embryologists confirm first-hand that the patient’s paperwork matches up with their egg, embryo, or sperm sample. In addition, a second embryologist confirms that the patient information matches.Once the team confirms identification for the retrieval, the physician surgically aspirates each follicle and the attending nurse will bring several vials from the operating room to the embryologist. The vials are—hopefully—filled with eggs. At the time of the retrieval though, the physician does not know exactly how many eggs he/she will obtain. If the patient is an egg donor, there could be upwards of 25 eggs obtained. If a woman is freezing her eggs or using her own eggs for fertility treatment, the quantity of eggs the physician retrieves can vary. The egg count is dependent upon factors like the woman’s age or the individual diagnosis.

The post-retrieval vials do not have a perfect egg that is ready to be fertilized, so an embryologist must examine the contents of each vial in a culture dish with an inverted microscope. Using a sterilized pipette, the embryologist hunts through the follicular fluid and blood, looking for the retrieved eggs. Once he/she finds the eggs, the count is marked down and told to the nurse. Then the eggs are put into media, specially designed and formulated to replicate in vivo conditions, and placed into an incubator.
Watch On-Demand: Inside the IVF Lab
- Vitrification
Vitrification is a revolutionary medical procedure that has changed fertility treatment. Embryo and egg freezing has been around for many years, but until recently it wasn’t always reliable. Embryologists had traditionally used a slow-freezing technology, called cryopreservation, which often allowed ice crystals to form inside the egg or embryo, thus damaging the eggs or embryos. Vitrification, a fast-freezing process, improved freezing exponentially.To perform vitrification, the embryologist will place the egg or embryo into freezing media droplets on a culture dish. Over the next 10 minutes, the egg or embryo undergoes serial exposure to an increasing concentration of cryo-protectant before it is loaded onto a straw. The straw is then rapidly dipped into liquid nitrogen for less than 1 minute. With that, vitrification is complete and the straw is put onto a cane and stored in a cryotank. Eggs and embryos can remain in the tank indefinitely.
The lab has an abundance of tanks full of clearly labeled eggs and embryos (to eliminate the possibility of identity confusion), largely due to vitrification’s growth in popularity. This is largely because of frozen embryo transfers ( FETs) success rates—which are now nearly identical to fresh embryo transfer rates—but also because of an increase in elective single embryo transfers (eSET) to reduce multiple pregnancies.
In addition to embryo freezing, many women freeze their eggs prior to undergoing chemotherapy treatment for cancer to preserve their current fertility—then return after treatment to use the eggs. This “stopping of the clock” helps as that later date may be otherwise considered advanced maternal age.
As with egg retrievals, the Shady Grove Fertility team performs a two-step identification confirmation before an embryo transfer can occur. An additional identification confirmation is done with the patient for this procedure. Early in the morning, the embryologists do an assessment of each transfer patients’ embryos, selecting the best possible one(s) for transfer.Once the embryologist selects the best embryo, he/she will go into the transfer room to identify the patient directly. All parties involved—the patient, embryologist, physician, and a witness—will verbally confirmed and sign off on the number of embryos the physician will transfer. Via ultrasound, the physician places the embryo(s) into the uterus. The embryologist then checks the catheter in the lab to make sure that there are no embryos remaining, thus confirming that there was a successful transfer. After the transfer, the patient will receive a picture of their embryo.For women that are returning to use previously frozen eggs, the embryologist will thaw and fertilize a select number of eggs. Same as with fresh eggs that have fertilized, the newly formed embryos will develop in the lab for typically 5 days prior to the embryo transfer.
Preimplantation genetic diagnosis (PGD) is a cellular biopsy looking for specific genetic diseases like cystic fibrosis or sickle cell anemia (to name a few). There are several reasons why a physician may recommend PGD:
- recurrent pregnancy loss
- recurrent in vitro fertilization (IVF) failure
- when the mother and father are known carriers of a genetic disease that they do not want passed on to their future child
The embryologist performs PGD in the lab preferably when the embryo has reached the blastocyst stage, meaning that the embryo is made up of several hundred cells. The embryologist removes about three cells from the embryo and sends them to an outside lab for testing. The turnaround time for testing is about 24 hours.
Learn more in Genetic Testing: Medical Miracle or Ethical Quandary?
- Sperm Wash

While SGF has a separate andrology lab that performs semen analyses, the embryology lab also has a sperm station. As with the eggs, the embryologists want to select the best possible sperm for IVF. On the day the woman is having her eggs retrieved, the sperm also needs to be obtained. The male partner will often bring a sample that he obtained in advance and it will be kept in the lab until it’s time for insemination. A woman may also use previously frozen sperm from the male partner or a donor that will be thawed for IVF.
At the sperm station, the andrologist will wash (separately) all sperm needed for that afternoon’s inseminations. After he/she washes the sperm, the good sperm will swim up in the sample, letting the embryologists know which ones are candidates for selection.
- Intracytoplasmic Sperm Injection (ICSI)

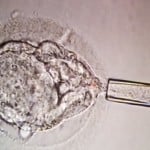
Intracytoplasmic sperm injection (ICSI) is a form of fertilization performed in the lab that differs from conventional fertilization. Conventional fertilization occurs when the embryologist places the male partner’s washed sperm directly on top of the egg and leaves it overnight. The embryologist brings together the highest quality egg and sperm and then lets them come together on their own. This doesn’t always work out though, particularly if male factor infertility is present. This is where ICSI comes in: an embryologist injects a single, healthy sperm into the cytoplasm, or center, of each egg. Since fertilization only requires one healthy sperm, ICSI has become one of the most transformational advances in fertility treatment.
ICSI, like conventional IVF, still needs the embryologist to select the best sperm from the already-washed sample. The embryologist will proceed to ‘catch sperm,’ using a pipette and microscope to identify the sperm he/she will use for insemination. It’s not just about who is the fastest swimmer, it’s largely about the morphology, or shape, of the sperm. The embryologist will grab the sperm by the tail and bring them onto a culture dish. It might take an embryologist up to an hour to find a single viable sperm. Once he/she obtains the sperm, it’s time to inseminate. The pipette enters the egg and the embryologist places a single sperm in the center. ICSI is a revolutionary treatment and has changed reproductive potential for couples experiencing severe male factor infertility.
The Importance of the Lab
All of the aforementioned technology is scientifically impressive, but why does it really matter? SGF is a center of excellence, a place where families begin and patients’ dreams become reality. Our success rates are remarkable and it’s largely due to our technology. But it’s more than the technology—it’s also the talented and dedicated embryologists who wield the technology. The machines would have no use without these men and women.





