At Shady Grove Fertility, we know that staying on the cutting edge of fertility research is the best way to provide you the best quality treatment available. Therefore, we make continual study and practice refinement among our top priorities.
“But not every new idea or new technique that you see on television or read about in a medical journal is a practical solution for couples trying to conceive a baby,” reminds Shady Grove Fertility Medical Director, Eric A. Widra, M.D. With new fertility innovations taking place all the time, how do you know what’s really available to you—or what will be available to you soon?
Knowing which options are viable and those that need further research can help you to determine your best course of action. Here’s your guide to what you should watch in fertility innovation and what’s not worth your time.
Watch: Preimplantation Genetic Screening (PGS)
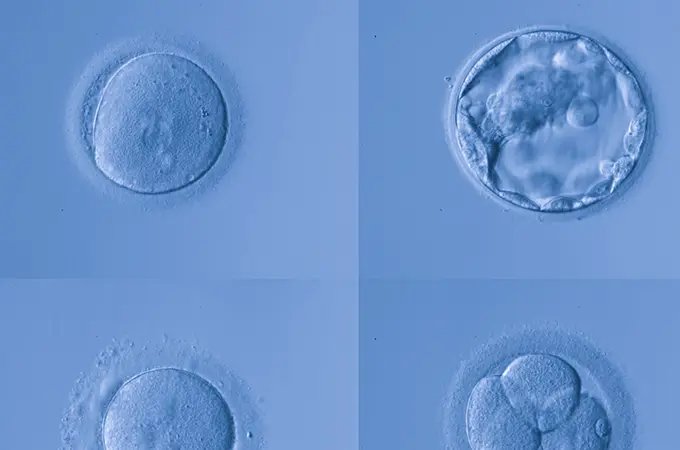
Preimplantation genetic screening (PGS) is the process of assessing embryo quality prior to implantation. While not a new practice, “people are increasingly using PGS,” says Dr. Widra. He continues, “Because of this screening, we’re no longer putting abnormal embryos into the uterus and can therefore increase pregnancy success rates.”
Dr. Widra continues, “Preimplantation genetic screening often results in a reduction in the pool of embryos from which a couple has to select. While this can be seen as a disadvantage, it is mitigated by the fact that the embryos that remain, while fewer in number, have a greater chance of successful implantation and eventual live birth.”
This procedure is similar to preimplantation genetic diagnosis (PGD). In PGS, however, fertility specialists assess only the number of chromosomes in the embryo. PGD, on the other hand, allows for the identification of specific genetic diseases or chromosomal abnormalities, including translocations.
Not: Sperm Generation
In 2016, researchers from the National Institute of Child Health and Human Development (NICHD) explored the feasibility of sperm development. While their findings seem promising—particularly for the approximately 30 percent of couples experiencing male-factor infertility, NICHD’s research has proven successful only in laboratory settings, not in real-world application.
“While it would certainly be beneficial to artificially produce sperm outside of the body, this technique won’t be coming to market soon and is not yet a dependable solution for patients seeking solutions for male infertility,” advises Dr. Widra.
Watch: Mini-IVF
Though highly effective, traditional in-vitro fertilization (IVF) requires expensive medications and a series of injections. Mini-IVF, or low-dose IVF, is an alternative that results in reduced costs and fewer injections.
“Because a woman is given less medication when using mini-IVF, she will produce fewer eggs per IVF cycle for extraction. For this reason, at Shady Grove Fertility, we don’t recommend mini-IVF as a front-line therapy for most as it is only truly beneficial for a select group of women,” adds Dr. Widra.
“We do think that there’s a role for Mini-IVF for women who are low responders, however,” says Dr. Widra. “Many naturally low responding women, or those who mature only a small number of eggs, will produce the same number of eggs no matter the dose of medication. Because the medication quantity makes no apparent difference in these women, the lower dose, which is part of the mini-IVF treatment, may be more appropriate,” says Dr. Widra.
Not: Stimulated Egg Production or Improvement
Egg quality can be an impediment standing between many couples and their dream of parenthood. Traditionally, the only solution for these women has been to seek an egg donor. Some reproductive medicine specialists have been working to create another option, dedicating their time to exploring potential methods of either inducing egg production in older women or improving the quality of aging eggs.
“Unfortunately, there has yet to be any positive findings to suggest that either is possible. Like medically-induced sperm production, most fertility experts believe that egg production or improvement as viable fertility treatment is far from practical application,” says Dr. Widra.
Watch: Three-Parent Embryos
“Through the use of three-parent embryo techniques, clinicians have been able to help women with mitochondrial diseases reproduce without worry. Doctors can fortify the women’s eggs with healthy mitochondria and, in doing so, prevent mothers from passing their potentially debilitating diseases on to their children,” adds Dr. Widra.
“While life-changing for those dealing with mitochondrial diseases, these diseases are quite rare, so the application of this technique is relatively limited,” Dr. Widra advises.
Some researchers have theorized that these techniques could also be used to improve the quality of older eggs, though this theory hasn’t been proven true. Additionally, the FDA does not support the use of this procedure for this purpose.
Not: In-Vitro Maturation (IVM)
Through IVM, doctors extract immature eggs from a woman’s ovaries and create an environment outside of the body in which the eggs can develop to maturity.
Gathering immature eggs departs from typical egg retrieval procedures. Generally, women are given medication that encourages eggs to mature in the body. The mature eggs are then retrieved and used for embryo development within a fertility center.
“Because medication can induce egg maturation within the body, however, this particular piece of reproductive technology is largely unnecessary. Additionally, while some research suggests that IVM is possible, many studies employ medications to stimulate the eggs to mature before removal. The use of these medications hampers the validity of the studies,” advises Dr. Widra.
“Proponents argue that IVM could be a cost-saving alternative to IVF, but we consider those cost savings to be minimal as the money saved on maturation-inducing medication is instead spent on lab procedures. Additionally, IVM is a cumbersome procedure for both women and fertility doctors,” adds Dr. Widra.
“Given advancements within the fertility community, inducing egg maturation within a woman’s ovaries is not particularly difficult. As a result, IVM, while theoretically possible, is more of a regression than a step into the future,” says Dr. Widra.
Watch: Fertility Preservation
To the benefit of women everywhere, it is now possible to take steps to preserve fertility, a process commonly known as egg freezing.
Women can undergo fertility preservation for elective reasons. Women who are aging but haven’t yet found a partner or are busy with their careers and wish to start their families later commonly take advantage of fertility preservation options.
Fertility preservation techniques are also increasingly used with women who face diseases that threaten their natural fertility. For example, women with cancer can preserve the possibility of a child despite cancer treatments, such as radiation or chemotherapy, that may decimate their fertility.
Presently, doctors can engage in fertility preservation in a number of ways. Most commonly, doctors stimulate the production of eggs as they would if they were going to perform IVF, and then freeze them.
“Recent medical innovations have also made it possible to harvest ovarian tissue as a means of collecting eggs. Because this procedure is more invasive and the stimulation of eggs has become quite easy, this technique is most often reserved for young or prepubescent girls who risk losing their fertility as a result of cancer or another medical condition. By gathering this tissue, doctors can use IVF treatment to allow young women facing cancer to become mothers in the future,” adds Dr. Widra.
“In the coming years, we expect the application of these techniques to increase. The success rates continue to climb as clinicians do more research and improve their skills and understanding of human reproductions,” says Dr. Widra.
A Bright Future in Fertility Innovation
“While the medical community has yet to refine techniques to the point where we can help every couple experiencing infertility successfully conceive, scientific advancements and medical technology continue to bring us much closer to this goal. As research continues into 2017 and beyond, we expect the frequency of success of fertility procedures in general, and the birth rate in particular, to continue to rise,” Dr. Widra adds.
At Shady Grove Fertility, we are dedicated to helping you on your path to parenthood. We offer a diverse set of procedures and work with couples to create customized plans, tailored to ensure the best possible outcomes for each set of prospective parents. Providing compassionate and comprehensive patient care is our practices’ top priority.

Medical contribution by: Eric A. Widra, M.D. of Shady Grove Fertility’s Washington, D.C. K Street Location
Infertility is a big mountain to climb alone. Let us partner with you and help you reach your goal of parenthood. For more information about advancements in infertility treatments, or to schedule an appointment with one of our New Patient Liaisons, please call 1-877-971-7755 or click here.
At Shady Grove Fertility, we’re here to give you the caring support you deserve as you start or grow your family. As a leading fertility and IVF center of excellence, we offer patients individualized care, innovative financial options, over 30 accepted insurance plans, and pregnancy rates among the highest of all national centers. We offer patients the convenience of 19 full-service and 6 satellite locations across Maryland, Pennsylvania, Virginia, and Washington, D.C. More than 1,700 physicians choose Shady Grove Fertility to refer their patients, and more than 96 percent of our patients say they would recommend Shady Grove Fertility’s 35+ physicians to a friend. With 10 Shady Grove Fertility babies born each day, your dream of starting or growing your family is within reach.