Medical contribution by Shruti Malik M.D.

For patients who are undergoing infertility treatment, the decision to change to a new treatment can spur anxiety, confusion, and uncertainty. How do you know when it’s time? Is this a decision your physician will make or will you work together to arrive at the best course of action? What are your options?
At Shady Grove Fertility, while it depends upon your diagnosis, we believe in a stepped approach to care, starting our patients with the simplest, most affordable treatment options first. Your physician will only recommend transitioning to a more advanced treatment if it is absolutely necessary—and you and your physician will make this choice together.
Moving to a Fertility Specialist
One of the most important transitions you can make is deciding to move from your OB/GYN to a fertility specialist. Fertility specialists typically have more experience diagnosing and treating infertility.
When you first visit your fertility specialist, you will undergo the basic infertility work-up for both partners. This diagnostic testing can provide key insights into your fertility. The female partner will have bloodwork performed, as well as an ultrasound. The bloodwork will measure for key hormones in determining ovarian function. The ultrasound will help to determine if the uterine cavity is normal. A woman will also need a hysterosalpingogram (HSG), which provides a view of the uterus and the tubes to ensure that there aren’t any blockages. The male partner will undergo a semen analysis to determine the sperm’s potential to fertilize the egg. Once the initial fertility work-up is complete and your physician also reviews your medical history, he or she will be able to determine a diagnosis and the course of treatment.
As mentioned earlier, many patients will begin with the simplest (or low-tech) treatment options first, but there are those who will move straight to in vitro fertilization (IVF). While there are many different factors that could lead to that treatment decision, one example of this is couples who have unexplained infertility. Studies concluded that intrauterine insemination (IUI) (a form of low-tech treatment) did not increase a couple’s chances of conception in comparison to when they were not undergoing treatment.[i] The patient would decide how they want to proceed though, knowing this information as well as their own personal diagnostics.

First-Line Therapies: Low-Tech Infertility Treatment
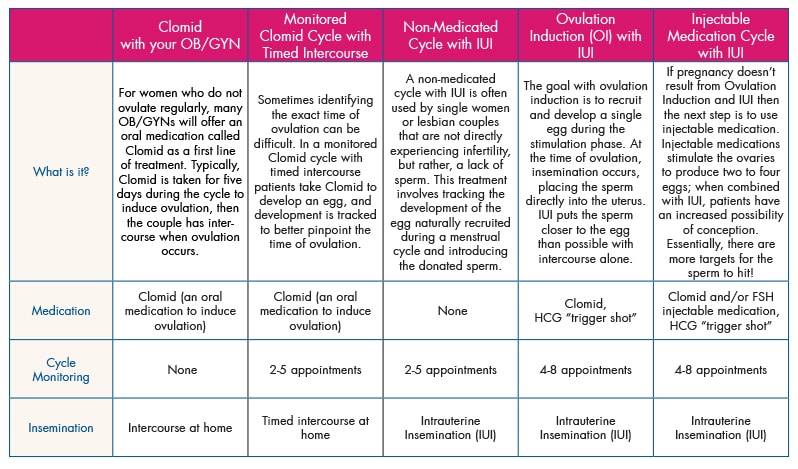
Physicians typically divide infertility treatments into low-tech treatments and advanced treatments. Low-tech infertility treatment options are what are known as “first-line therapies.” These options aim to develop one to four eggs, with fertilization occurring within the woman’s body rather than the laboratory setting.
Five low-tech treatment options used by patients are:
- Clomiphene citrate (clomiphene, Clomid, Serophene) with your OB/GYN
- Clomid (an oral medication that helps treat irregular or absent ovulation) is often the first-line therapy for many women, usually while under the care of their OB/GYN. While it can definitely prove successful for some women, how do you determine if you’ve taken Clomid for too long? The data for Clomid shows that after three to four cycles, the success rates drop off dramatically, even if the woman is ovulating.[ii] If she is over 35 or the couple’s infertility is unexplained, the data show that they should move on even sooner. It has actually been shown that it is more cost effective to switch to advanced treatments, rather than continue with Clomid after three to four cycles.
- Monitored Clomid cycle with timed intercourse
- If you started Clomid with your OB/GYN and have since transitioned to a fertility specialist, your physician may decide to continue with Clomid along with monitoring with bloodwork and ultrasound. You would come to the office for two to five monitoring appointments, in order to better pinpoint when ovulation may be occurring.
- Non-medicated cycle with IUI
- This treatment can be used by couples who do not want to use Clomid or other medications, or who may have mild male factory infertility present. IUI places the sperm in the upper portion of the uterus, and thus, closer to the egg. IUI is also often used by single women or same sex couples who are using donor sperm.
- Ovulation induction (OI) with IUI
- In ovulation induction with IUI, Clomid is used to induce ovulation. IUI with Clomid can be useful because Clomid can have an effect on cervical mucus by making it thicker and harder for sperm to penetrate. The IUI bypasses this issue by directly placing the sperm in the upper portion of the uterus.
- Injectible medication cycle with IUI
- An injectible medication cycle can be used for women who may have diminished ovarian reserve or certain hormonal disorders, rendering Clomid relatively ineffective.
If a treatment cycle does not result in a pregnancy, you will meet with your physician to review your cycle and discuss how to proceed. Your physician will provide information about the success rates and other available data so that you can make the most informed decision about a possible treatment transition.
Deciding to Transition to IVF
For the majority of patients, success rates for IUI will drop off after three unsuccessful cycles. If a couple is young and they want to try a fourth cycle of IUI, a physician will likely support this decision, depending on the individual diagnosis. But for couples in which the woman is over the age of 35, there is a correlation between the decline in success rates and advanced age. This is usually when your physician will advocate switching treatments to IVF.
IVF is the most successful treatment a couple can do using their own eggs and sperm. It is also one of the few treatment options in which success rates have increased over time due to technological advances. In 2013 at Shady Grove Fertility, women under 35 had a 48 percent live birth rate per embryo transfer and women 35 to 37 had a 43 percent live birth rate per embryo transfer.[iii]
Additionally, many women undergoing IVF will have remaining high-quality embryos to freeze for future frozen embryo transfers (FET), providing patients with many chances for success or the ability to return for additional children later on.
When Donor Egg Treatment is Necessary
Women who are unable to use their own eggs for conception, but can still carry a child in their uterus, may need donor egg treatment. A physician may recommend donor egg treatment for women who have decreased ovarian function, premature ovarian failure, or genetic abnormalities. The majority of women who undergo donor egg treatment, though, have usually tried other infertility treatments that were unsuccessful.
Donor egg treatment offers the highest pregnancy and delivery rates of any fertility treatment, as the donated eggs come from women between the ages of 21 and 32, which coincides with a woman’s peak fertility. In 2013, donor egg recipients at Shady Grove Fertility had a 58 percent clinical pregnancy rate per embryo transfer and a 49 percent live birth rate per embryo transfer. [iv]
Knowing Your Options
Low-tech infertility treatment, IVF, and donor egg treatment represent the full course of care options available for infertility treatment. It is unlikely that most patients will need all of these options, but it is important to be aware that they exist and to let them guide you in your decisions about treatment transitions. If you are considering another form of treatment, consider how many cycles you have attempted, your age, and the guidance from your medical team based on their data-driven decisions. Consider the statistics, but also do what feels right for you and your family.
For more information about infertility treatment or to schedule an appointment with one of our physicians, please speak with our New Patient Center at 888-761-1967.
References:





